For the past several years, Ukraine has pursued comprehensive health reform, aiming to improve health the outcomes of its citizens, increase the health system’s efficiency, and provide financial protection from high out-of-pocket payments. This reform included massive changes in health financing, decentralization, rationalization of institutional and government roles, procurement reform, changes to pharmaceutical management, and increased opportunities for private sector engagement in the health system.
A facet of this effort has been the development of telemedicine to strengthen transparency and efficiency in the health sector, reduce opportunities for corruption, and expand access to quality health services. Telemedicine has become a critical tool to maintain Ukrainians’ access to health care since the Russian full-scale invasion in February 2022.
LHSS works with the USAID mission in Kyiv and the Government of Ukraine (GOU) to establish the foundation for institutional arrangements and capacity to govern and ensure telemedicine is safely and sustainably offered to the population. The project also works with the Ministry of Health to rapidly deploy telemedicine solutions to ensure Ukrainians’ uninterrupted access to health services.
Approach
LHSS is working closely with government stakeholders and local partners to achieve the following objectives:
- Strengthen telemedicine governance, policies, and financing by generating knowledge of telemedicine in Ukraine to inform the GOU’s decision-making, supporting the creation and implementing of a shared national vision for telemedicine development, and defining financing and purchasing arrangements.
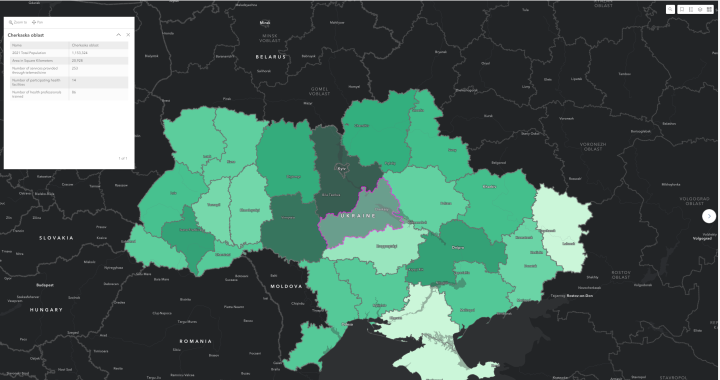
- Advance equitable and sustainable access to health services by accelerating access to telemedicine among vulnerable groups, identifying synergies with local private sector entities to expand telemedicine reach, and designing an enabling environment for telemedicine systems to be interoperable with the eHealth system.
- Strengthen the GOU’s capacity for managing offers to use private sector telemedicine solutions during wartime and rapidly implement these solutions to meet Ukrainians’ urgent health needs.
Progress Highlights
- LHSS, in coordination with the eHealth state-owned enterprise, helped the MOH create a standardized approach, approved by the MOH in July 2022, to evaluate offers of telemedicine solutions so that all accepted donations would integrate well into Ukraine’s health system.
- LHSS strengthened the MOH’s capacity to partner with the private sector, resulting in successfully leveraging telemedicine solutions and equipment donated by private companies valued at $3.5 million.
- Recognizing the fragmented nature of telemedicine governance, LHSS worked closely alongside the MOH to create and facilitate the country’s first interagency working group focused on expanding access to telemedicine. Convening private and public sector stakeholders, the group created a strategy and operations plan that provide a shared vision, principles, and direction for telemedicine development in Ukraine.
-
With LHSS support, the MOH introduced a draft law that provides a legal foundation for the broader use of telemedicine services in medical care and rehabilitation. The draft was approved by the Government of Ukraine in July 2023 and later signed into law in September 2023. Vox Ukraine, an independent analytical platform focused on economics, governance, and social developments in the country, recognized the law as reformative in November 2023.
- Since the inception of the activity in FY22 to date, LHSS has engaged a total of 324 facilities. In sum, these facilities have provided 6,098 services to patients using telemedicine solutions donated to Ukraine as humanitarian aid and supported by LHSS as requested by the MOH. To ensure high-quality service provision and appropriate utilization of telemedicine solutions, LHSS trained 564 service providers and conducted 756 technical support sessions
- Implementation of the tele-health Rehabilitation Gaming System (RGS), developed by Eodyne, which allows doctors to create individual rehabilitation plans for patients who, due to conflict and hostilities, may have limited access to traditional health care.